|
|
RevNet User Guide - Payer Verification |
|
|
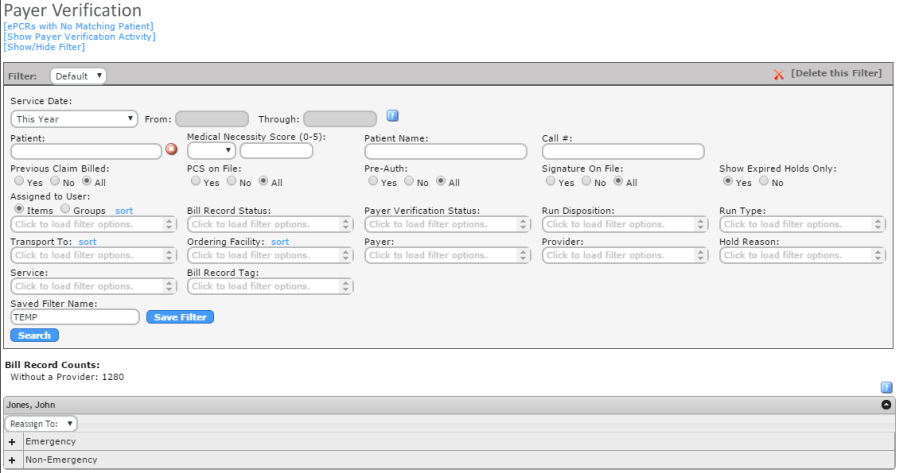
Payer Verification |
|
|
Navigate to: Finance -> Payer Verification |
||
|
Payer Verification Overview |
||
|
Payer Verification page is used to confirm payers are correct and eligibility is checked prior to billing. |
||
|
The Payer Verification Page can be filtered by Service Date, Medical Necessity Score (0-5), Patient Name, Call #, Previous Claim Billed (Yes, No, All), PCS on File (Yes, No, All), Pre-Auth (Yes, No, All), Signature on File (Yes, No, All), Show Expired Holds Only (Yes, No), Assigned to User, Bill Record Status, Payer Verification Status, Run Disposition, Run Type, Transport To, Ordering Facility, Payer, Provider, Hold Reason, Service and/or Bill Record Tag. |
||
|
|
||
|
[ePCRs with No Matching Patient]: Click here to navigate to the Patient Matching Page. |
||
|
Bill Record Counts: |
||
|
Without a Provider: Number of Bill Records that do not have a provider assigned. |
||
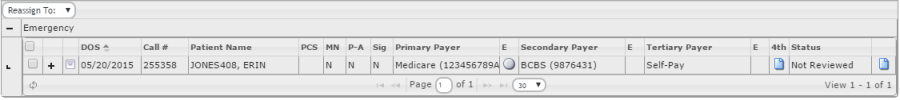
| Payer Verification Details | ||
|
|
||
|
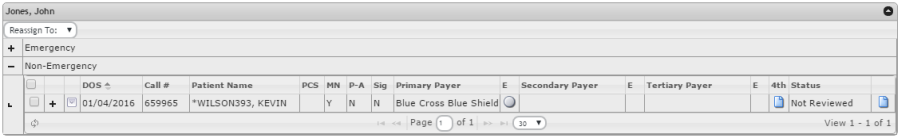
Service Date: Service Date of the Call |
||
|
Call #: Call # for the Call, as assigned in the Match ePCR to CAD Page |
||
|
Patient Name^Last Claim Generated: Patient Name, as assigned on the Match eCPR to Patient Page. Hover over the Patient Name to see the last claim generated date. |
||
|
PCS: Indicator (Y/N) of if the patient has the Physician Certification Statement. |
||
|
MN: Indicator (Y/N) of if the call was calculated as Medically Necessary. |
||
|
P-A: Indicator (Y/N) if the patient has a Prior-Authorization. |
||
|
Sig: Indicator (Y/N) if the Patient has a Signature on File. |
||
|
Payers/E: The list of payers for the patient. If Insurances are not in the correct order, click in the line and use the Drop Down list to update and click Save. Click the to check eligibility for the patient/insurance. |
||
|
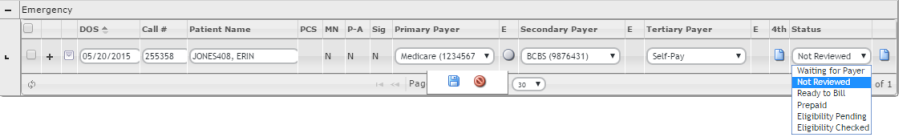
Status: Statuses
include Not Reviewed, Waiting for Payer, Ready to Bill and Hold
Statuses setup under Setup -> RevNet -> Hold Reasons. To update
the Status, click in the line and use the drop down list to
select the appropriate status. Click
|
||
|
Comment: Click to add a comment to this call. |
||
|
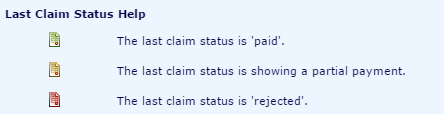
LCS: Last Claim Sent status. If Blank, there has been no previous claim. Last Claim Status icon is green, last claim was paid. If yellow, claim was partially paid. If red, claim was rejected. |
||
|
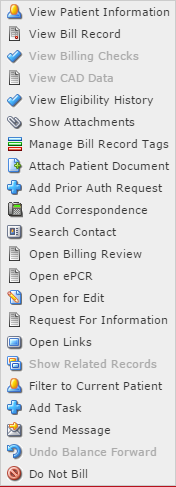
Action Item List |
||
|
The Action Item List is available for
all Bill Records. Click |
||
|
|
||
|
View Patient Information: Opens Patient Information page. Click HERE for more information on Patient Information. |
||
|
View Bill Record: Opens the Bill Record page. Click HERE for more information on Bill Records. |
||
|
View Billing Checks: Opens the Billing Checks page for this call #. This will only be enabled if the Status is Ready to Bill. |
||
|
View CAD Data: Opens the CAD Data page that is associated with this call. |
||
|
View Eligibility History: View the Eligibility History for the call. This will only be enabled if the agency is contracted with Zirmed for eligibility checks. |
||
|
Show Attachments: Shows documents that have been attached to the ePCR. |
||
|
Manage Bill Record Tags: Add/Edit/View Tags for this bill record. Tags are ways to group bill records. |
||
|
Attach Patient Document: Attach Document is not currently supported and will be included in a future release. |
||
|
Add Prior Auth Request: Select if payer requires Prior Authorization. |
||
|
Add Correspondence: Add Correspondence will allow for adding a correspondence with the patient regarding this call. |
||
|
Search Contact: Shows all correspondence added for this call and allow for searching these correspondences. |
||
|
Open Billing Review: Opens the Billing Review report for this call. |
||
|
Open ePCR: Opens the Prehospital Care Report Summary for this call. |
||
|
Open for Edit: Opens the ePCR and allow for edits. |
||
|
Request for Information: Opens the Request for Information report to be sent to the patient to obtain more information regarding insurances. |
||
|
Open Links: Opens the General Payer Verification Links page. These links have been previously setup under Setup -> RevNet -> External Links |
||
|
Show Related Records: Shows the other ePCRs/CAD Data that this call has been grouped to. |
||
|
Filter to Current Patient: Will search the Payer Verification Page for other Bill Records for this Patient. |
||
|
Add Task: Allows for a task to be added and assigned to a HealthEMS User. |
||
|
Send Message: Opens Add Message page to send a myMessage to a HealthEMS user. |
||
|
Undo Balance Forward: Will Undo the most current Balance Forward that has been completed for this call. Balance Forward will be discussed in the AR Management -> Cash Receipts section of the User Guide. |
||
|
Do Not Bill: Marks the Bill Record as Do Not Bill. |
||
|
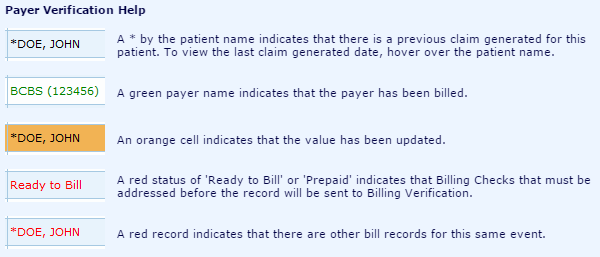
Payer Verification Help |
||
|
|
||
|
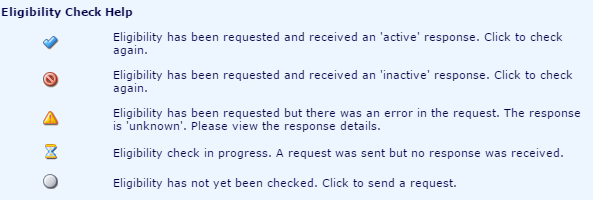
Eligibility Verification Help |
||
|
|
||
|
Last Claim Status Help |
||
|
|
||
|
Bill Record Overview |
||
|
Click HERE For an overview of the Bill Record. |
||
|
Update Status |
||
|
To update the Status of
a call, click within the line. Use the Status
drop down list to select the requested status and click
|
||
|
|
||
|
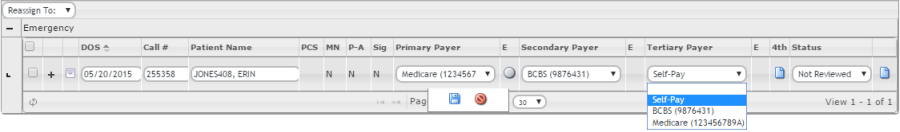
Update Payers |
||
|
To update the Primary Payer,
Secondary Payer and/or Tertiary Payer of
a call, click within the line. Use the Payer drop
down lists to update the payers and click |
||
|
|
||
|
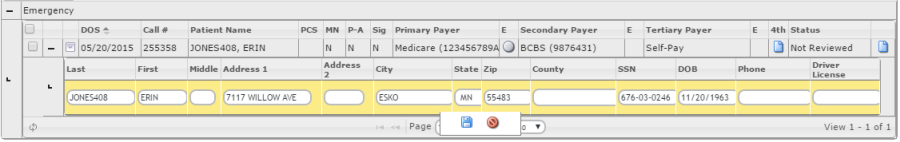
Update Patient Information |
||
|
Patient Information can also be updated from this page. To update patient, click +. |
||
|
|
||
|
Once the Patient information can be
seen, click within the line to enable the fields. Make changes
as needed and click
|
||
|
|
||
|
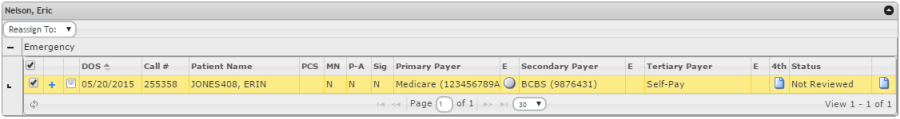
Re-assign Payer Verification Bill Records |
||
|
Payer Verification Records can be reassigned to other HealthEMS User. Check the box next to the Bill Record and use the "Reassign To:" Drop Down list to select the user. Records will be updated once the user is selected. |
||
|
|
||